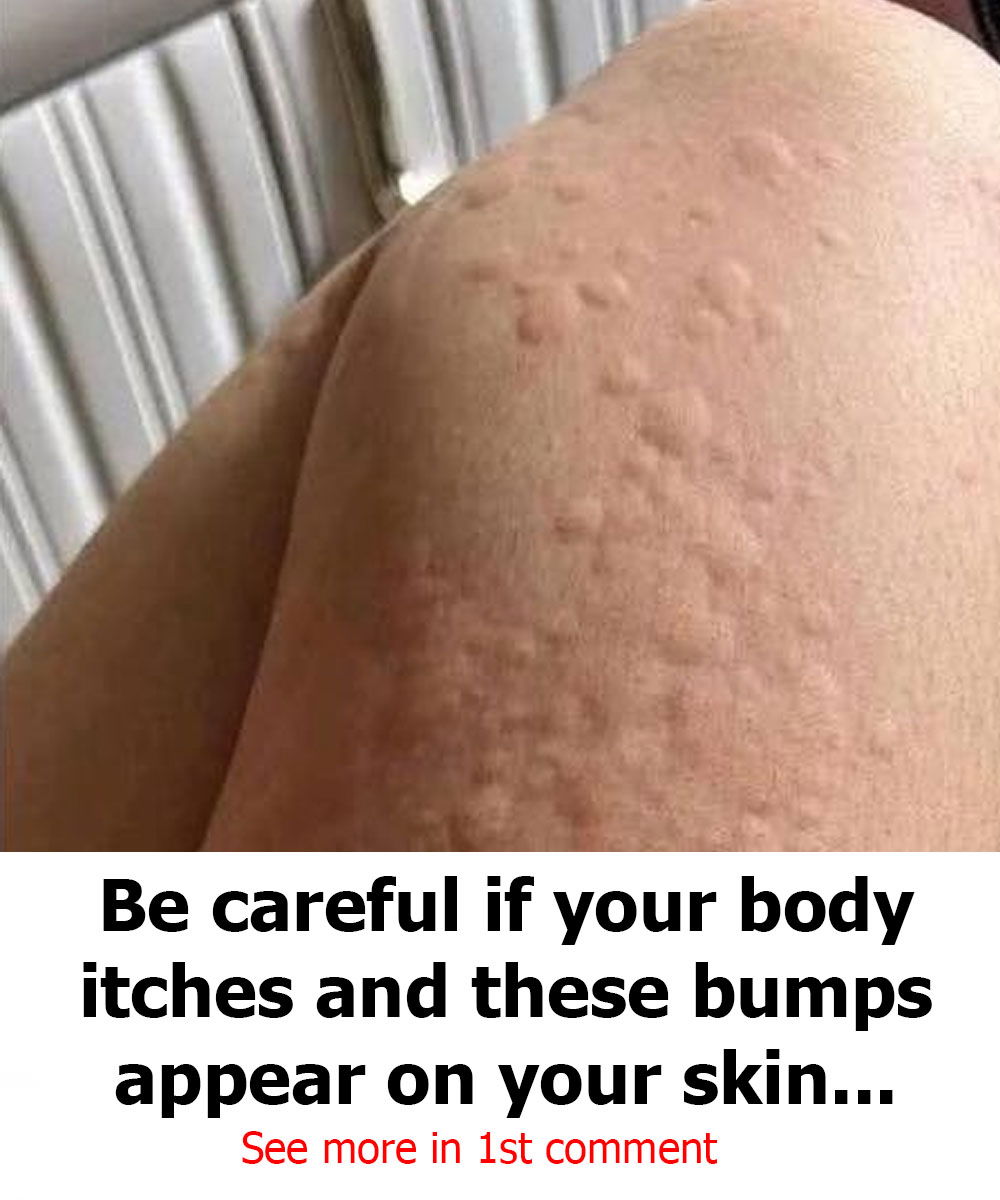
Urticaria is a skin condition characterized by the appearance of raised, red, itchy welts. These lesions can vary in size and form clusters that appear on various areas of the body, such as the face, arms, legs, and trunk. Although the welts usually disappear on their own after a few hours or days, in some cases they can recur, significantly affecting the well-being and quality of life of those who suffer from it.
Urticaria is a common and often disconcerting skin reaction that manifests as the appearance of welts or bumps on the skin. These lesions, which can range in size from small spots to large plaques, are characterized by being raised, red, or skin-colored, and typically intensely itchy. Although it can be alarming, in most cases, urticaria is a benign and transient condition.
Urticaria occurs when certain cells in the body, called mast cells, release histamine and other chemical mediators into the bloodstream. This release causes the small blood vessels in the skin (capillaries) to leak fluid, resulting in the formation of the characteristic edematous (swollen) welts.
The main symptoms of urticaria include:
Hives: Raised, well-circumscribed lesions that may be pale in the center and red at the edge.
Pruritus: Itching that can range from mild to very intense.
Evanescent Character: One of the most distinctive characteristics is that individual welts usually disappear in less than 24 hours without leaving a mark, although new ones may appear on other areas of the body.
In some cases, urticaria may be accompanied by angioedema, a swelling of the deeper layers of the skin. Angioedema commonly affects the eyelids, lips, hands, feet, or genitals and can cause a feeling of tightness or pain. If angioedema affects the throat or tongue, it can make breathing difficult and is considered a medical emergency.
Types of Urticaria

Urticaria is primarily classified according to its duration:
Acute Urticaria: This is the most common form. Outbreaks last less than six weeks, and the cause is often identifiable.
Chronic Urticaria: Diagnosed when outbreaks persist for more than six weeks. In many cases of chronic urticaria, the specific cause is difficult to determine, which is known as chronic spontaneous (or idiopathic) urticaria.
In addition, there is inducible or physical urticaria, in which the hives are triggered by a specific external stimulus, such as:
Dermographism: The appearance of hives when scratching or rubbing the skin.
Cold Urticaria: Triggered by exposure to cold.
Pressure Urticaria: Caused by sustained pressure on the skin (e.g., by tight clothing).
Solar Urticaria: Induced by exposure to sunlight.
Cholinergic Urticaria: Related to an increase in body temperature, such as during exercise or a hot bath.
Common Causes of Urticaria

The range of possible triggers for acute urticaria is wide:
Allergic Reactions: To foods (such as shellfish, nuts, eggs, and milk), medications (antibiotics, pain relievers such as aspirin or ibuprofen), insect bites, or latex.
Infections: Both viral (such as the common cold or hepatitis) and bacterial (strep throat).
Physical Factors: As mentioned for inducible urticaria.
Emotional Stress: Although not a direct cause, it can exacerbate outbreaks in susceptible individuals.
In chronic urticaria, an external cause is often not found. In a significant percentage of these cases, the cause is believed to be autoimmune, meaning the body’s own immune system attacks mast cells.
Diagnosis and Treatment
The diagnosis of urticaria is based primarily on the patient’s physical examination and medical history. The doctor will try to identify the duration of the outbreaks and possible triggers.
Treatment is primarily aimed at relieving symptoms and, if possible, avoiding triggering factors:
Antihistamines: These are the mainstay of treatment. They block the action of histamine, reducing itching and hive formation. Both over-the-counter and prescription antihistamines are used.
Corticosteroids: In more severe or persistent cases, oral corticosteroids may be prescribed for a short period to reduce inflammation.
Avoid Triggers: If a specific trigger has been identified, such as a food or medication, the most important measure is to avoid it.